Table of Contents
7 Reasons Why you need to Have Vitamin D
What is vitamin D, and how do we get it?
Vitamin D, “the sunshine vitamin” is a fat-soluble vitamin that is required by the body. It is considered both a hormone and a vitamin because, as per the traditional definition of a hormone (a substance made in one part of the body that exerts its effects on another part of the body), vitamin D fits the bill. We can obtain vitamin D by both conversion of ultraviolet (UV) (sun) light on our skin to pre-vitamin D as well as from food (see the Table for food sources of vitamin D). Note that fortified foods provide most vitamin D in the U.S. diet (4,5). Furthermore, at a northern latitude of approximately 42 degrees (northern border of California and Boston), there is no conversion to pre-vitamin D on the skin from UV light from November through February (6), and farther north, this can extend for 6 months.
In addition to the latitude, complete cloud cover can decrease the UV energy by approximately 50%, and shade can decrease it by 60%, which includes shade produced by pollution (7). Ultraviolet light does not infiltrate glass, and thus, if a person is exposed to sunlight indoors, there will be no conversion to pre-vitamin D on the skin from UV light (8).
Because of the increasing use of sunscreens to protect against skin cancers, conversion to pre-vitamin D on the skin from UV light is lessened (with a protection factor of 8 or more, conversion to pre-vitamin D does not take place). Nonetheless, most people do not usually apply adequate amounts of sunscreen, do not always cover all parts of their body, and generally do not reapply sunscreen regularly, and thus, some conversion to pre-vitamin D on the skin will probably occur (9).
Although vitamin D is important for health, providing guidelines for the amount of sun exposure is difficult, because of conflicting research on the needs for vitamin D and the need to prevent skin cancer. Some suggest, however, that approximately 5 to 30 minutes of sun exposure between 10 a.m. and 3 p.m. at least two times per week (face, arms, legs, or back) without sunscreen should provide enough pre-vitamin D production on the skin, which will lead to increased vitamin D synthesis within the body. Those individuals with limited sun exposure require good food sources of vitamin D and may need to supplement their diet with vitamin D (10,11).
No matter how vitamin D is acquired, from UV (sun) light, food, and/or supplements, vitamin D is inactive and must go through two hydroxylations in the body to become active. “Hydroxylation” simply means that hydroxyl (OH) groups are added to the structure of vitamin D. The first hydroxylation of vitamin D occurs in the liver, where vitamin D becomes 25-hydroxyvitamin D (25(OH)D), also identified as calcidiol. The second hydroxylation occurs in the kidney to become the most active form of vitamin D, 1,25-dihydroxyvitamin D [1,25(OH)2D], also known as calcitriol (12) (Figure).
FORMS OF VITAMIN D
Ergocalciferol is vitamin D2 and is found in plants, fungi, molds, lichen, and the like. It does not naturally occur in animals. Vitamin D3 (cholecalciferol) is widely distributed in animal tissues, fish oils, and fortified foods. It was once thought that vitamins D2 and D3 were physiologically equivalent; however, present data support that vitamin D3 is more metabolically active than vitamin D2 (13).
CURRENT DIETARY REFERENCE INTAKES FOR VITAMIN D
The current Dietary Reference Intake for vitamin D ranges from 200 international units (IU) per day for children to 600 IU/day for individuals older than 70 years (5). The Tolerable Upper Intake Level (UL) for vitamin D is 2,000 IU/day (5). Note that these Dietary Reference Intakes were established as Adequate Intakes for vitamin D, not Recommended Dietary Allowances, meaning that there was not sufficient scientific evidence available to establish the Recommended Dietary Allowances (5).
NORMAL BLOOD LEVELS OF VITAMIN D
At present, sufficient blood levels of vitamin D (measured by assessing 25(OH)D concentrations) are from 40 to 100 nmol/L; however, some have suggested that desirable serum levels of vitamin D, to maintain health and prevent certain diseases, should range from 75 to 160 nmol/L. To maintain sufficient concentrations of vitamin D, it has been suggested that individuals would require a vitamin D intake of 1,000 to 4,000 IU/day (a range that is mostly above the UL for vitamin D intake). To maintain desirable concentrations of vitamin D in the blood, it has been suggested that people would require an intake of 4,000 to 10,000 IU/day, which is above the UL for vitamin D (14).
VITAMIN D’S ROLE IN REGULATING CALCIUM WITHIN THE BODY
Normal levels of serum (blood) calcium range from 9 to 11 mg/dL; the body maintains tight regulation of serum calcium concentrations with three “calciotropic” hormones: parathyroid hormone, vitamin D, and calcitonin (15). When blood calcium concentrations fall below 9 mg/dL, parathyroid hormone sends a signal to increase the production of calcitriol in the kidneys. The increased concentrations of calcitriol in the body will lead to the following: increased renal (kidney) reabsorption of calcium-that is, less calcium will be lost in the urine; increased intestinal absorption of calcium-that is, more calcium will be absorbed by the small intestines, which is accomplished by the increased production of calbindin, a vitamin D-dependent protein that binds to calcium within the intestines for increased calcium absorption), and increased osteoclastic activity in the bones (greater bone breakdown), which releases calcium into the blood, until calcium balance is achieved. When blood calcium concentrations increase above 11 mg/dL, a hormone, calcitonin, will cause just the opposite to happen: decreased renal reabsorption of calcium, decreased intestinal calcium absorption, and increased osteoblastic activity (greater bone deposition).
Aside from its most famous role in calcium regulation, vitamin D has a number of other functions in the body. These include: bone metabolism, regulation of cell production and differentiation, protein synthesis, and improved muscle function (16).
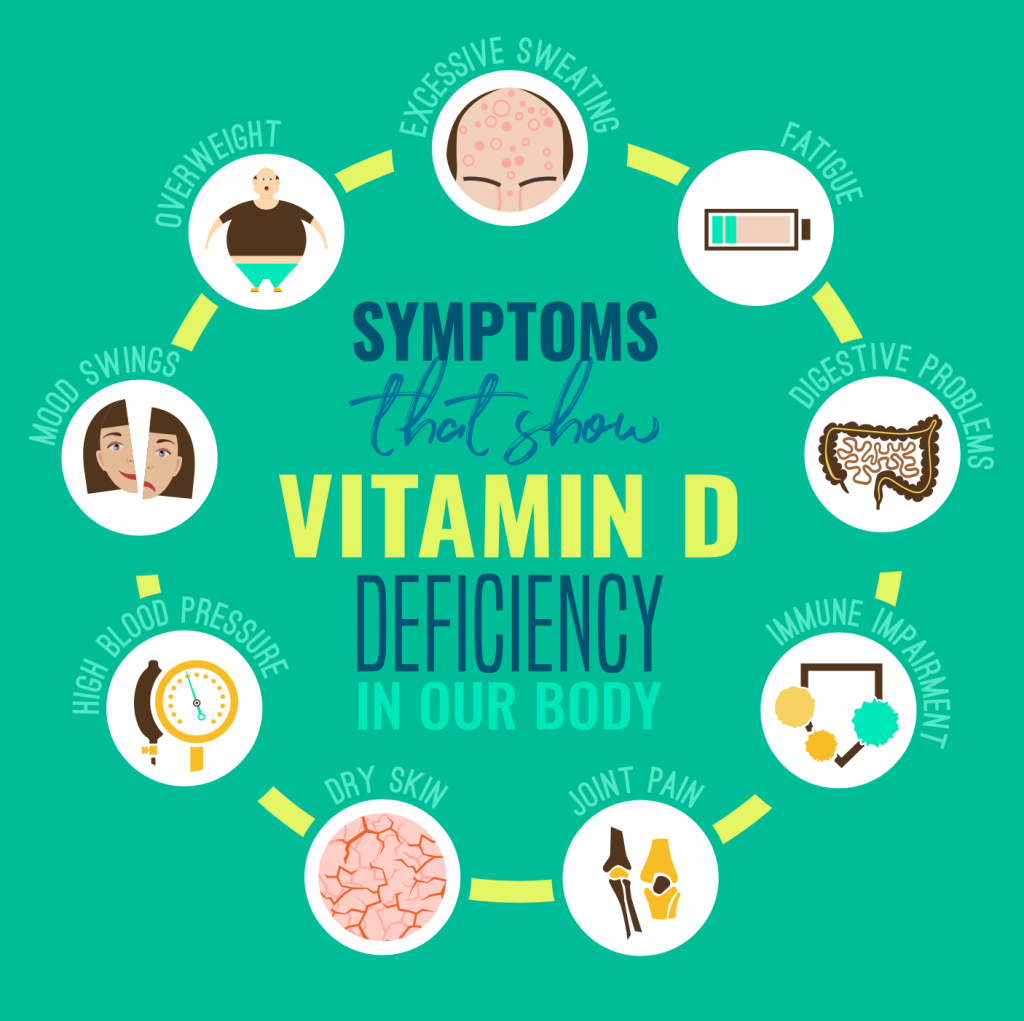
VITAMIN D DEFICIENCY
Rickets or osteomalacia (softening of the bones) is a direct result of vitamin D deficiency. Rickets occurs in childhood and osteomalacia in adulthood. Symptoms include bowed legs and muscle weakness. For people who live at 42 degrees latitude or above, combined with an increased use of sunscreen for cancer prevention, osteomalacia may become more common again.
SUMMARY
Vitamin D is a fat-soluble vitamin that also is a hormone. Vitamin D plays a major role in calcium regulation and bone metabolism. Vitamin D can be obtained by UV (sun) light and from foods. It seems that to maintain normal serum levels of vitamin D in the blood, dietary intake may need to be increased, but more research is required before definitive advice can be provided.
References
1. Pennington, J.A., and J.S. Douglass. Bowes and Church’s Food Values of Portions Commonly Used. 18th ed. Philadelphia: Lippincott Williams & Wilkins, 2004.
2. Nutrition Coordinating Center. Nutrition Data System for Research (NDS-R). Version 4.06/34. Minneapolis: University of Minnesota, 2003.
3. U.S. Department of Agriculture, Agricultural Research Service. USDA Nutrient Database for Standard Reference, Release 16. Nutrient Data Laboratory Home Page, 2003. Available at http://www.ars.usda.gov/main/site_main.htm?modecode=12354500.
4. Calvo, M.S., S.J. Whiting, and C.N. Barton. Vitamin D fortification in the United States and Canada: current status and data needs. The American Journal of Clinical Nutrition 80:1710S-1716S, 2004.
5. Food and Nutrition Board of the Institute of Medicine. Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington: National Academy Press, 1997.
6. Cranney, C., T. Horsely, S. O’Donnell, et al. Effectiveness and safety of vitamin D. Evidence Report/Technology Assessment No. 158 prepared by the University of Ottawa Evidence-based Practice Center under Contract No. 290-02.0021. AHRQ Publication No. 07-E013. Rockville: Agency for Healthcare Research and Quality, 2007.
7. Wharton, B., and N. Bishop. Rickets. Lancet 362:1389-400, 2003.
- Cited Here |
- PubMed | CrossRef
8. Holick, M.F. Photobiology of vitamin D. Vitamin D. Volume I. 2nd ed. Feldman, D., J.W. Pike, and F.H. Glorieux (Editors). Burlington: Elsevier, 2005.
9. Wolpowitz, D., and B.A. Gilchrest. The vitamin D questions: how much do you need and how should you get it? Journal of the American Academy of Dermatology 54:301-317, 2006.
10. Holick, M.F. Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health. Current Opinion in Endocrinology, Diabetes, and Obesity 9:87-98, 2002.
11. Holick, M.F. Vitamin D deficiency. The New England Journal of Medicine 357:266-281, 2007.
12. DeLuca, H.F. Overview of general physiologic features and functions of vitamin D. The American Journal of Clinical Nutrition 80:1689S-1696S, 2004.
13. DeLappe, E., C. McGreevy, N. ni Chadhain, et al. Vitamin D insufficiency in older female community-dwelling acute hospital admissions and the response to supplementation. European Journal of Clinical Nutrition 60(8):1009-1105, 2006.
14. Veith, R. Pharmacology of Vitamin D, Including Fortification Strategies. Vitamin D. 2nd ed. Feldman, D., and F. Glorieux (Editors). Toronto, Ontario, Canada: Elsevier, 2005.
15. Volpe, S.L., Vitamins, minerals, and exercise, in Sports Nutrition: A Practical Manual for Professionals. 4th ed. Dunford, M. (Editor). Chicago: The American Dietetic Association, 61-93, 2006.
16. Holick, M.L. Vitamin D. Modern Nutrition in Health and Disease. 10th ed. Shils M.E., M. Shike, A.C. Ross, et al. (Editors). Philadelphia: Lippincott Williams & Wilkins, 376-395, 2006.