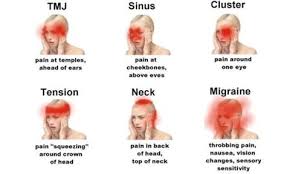
1 A pain by any other name. Most headaches tend to be grouped by their symptoms into three common categories-tension, migraine, and cluster. Unfortunately, the misery of headache pain will affect three of four people at least once a year. Even more troubling is the fact that headaches are a chronic problem for more than 45 million Americans.
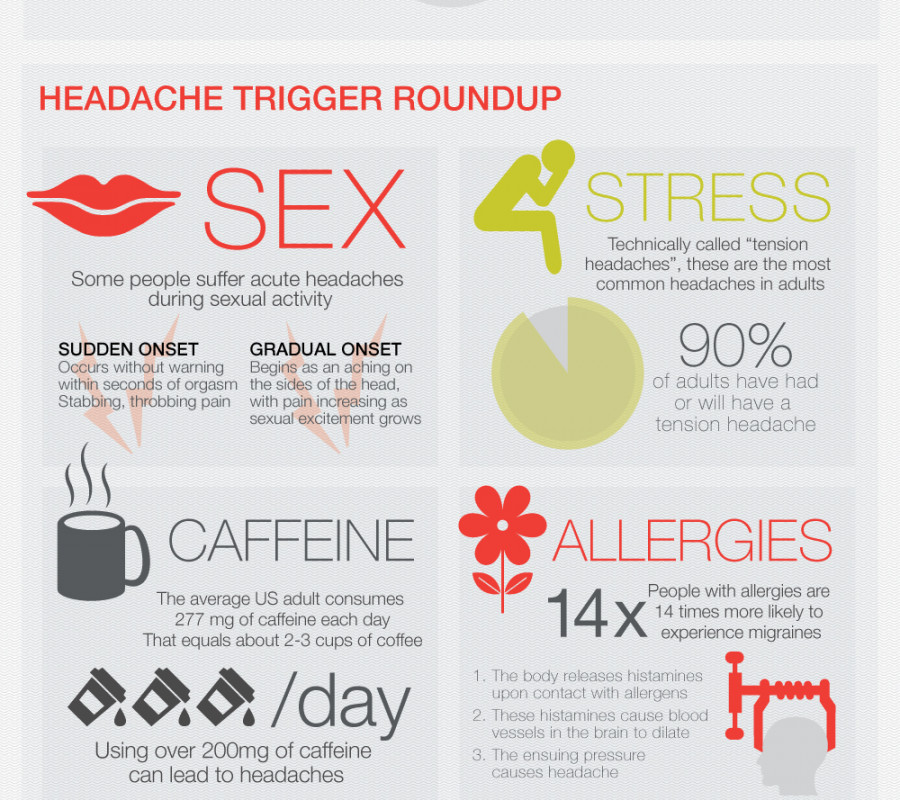
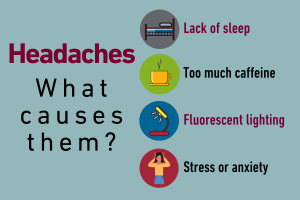
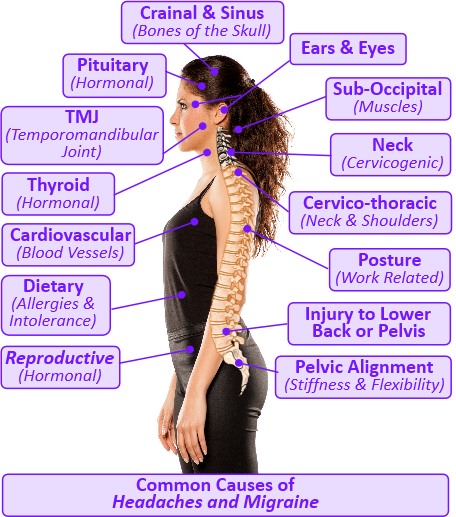
2 Cause and effect. In reality, the physiological causes of the most common types of headaches are not fully understood. At this time, no known cures exist for these debilitating and painful occurrences. What is known is that specific factors (including exercise) may create the conditions that lead to headaches in individuals who have a propensity for having such maladies.
3 Villain or hero? Exercise can be either a trigger or a treatment for headaches, depending on the type of headache and whether the exercise is properly prescribed. In this regard, avoiding the kind of physical activity regimen (e.g., acute, intense bouts) that can lead to headaches is essential. The key is for individuals to only engage in exercise that is appropriate for them.
4 Exercise is medicine. Engaging in aerobic exercise on a regular basis has been found to decrease the number of headaches that people experience and the severity of the episodes by as much as 50% because of its effect on the body’s release of endorphins and serotonin into the bloodstream. In this regard, it is essential that individuals who are prone to headaches increase their activity levels gradually over time, adequately warm-up, and cool down before and after exercising.
5 Stress and strain may lead to pain. Individuals who have tension-type headaches often report the onset of such headaches after strength training. It is important that these individuals while lifting weights, should always exercise through a full range of motion, avoid holding their breath, and overexerting themselves while exercising.
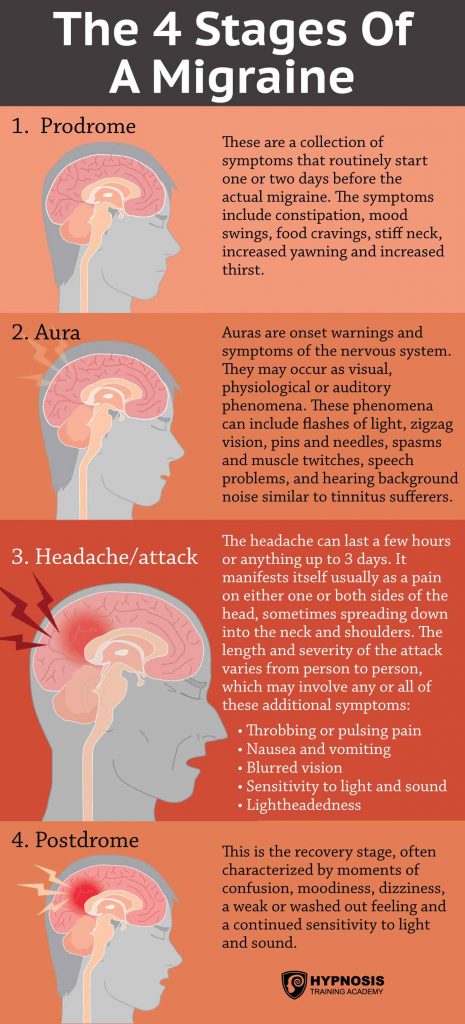
6 Exercise-induced migraines. Although the root causes of a migraine headache remain a mystery, migraine pain seems to come from inflammation and dilation of the blood vessels. Conventional wisdom dictates that migraine-prone individuals should consider taking an anti-inflammatory medication before working out and take particular care to ease into their exercise bout.
7 Safety first. On very rare occasions, headaches are symptomatic of a more serious problem. As such, individuals should make sure that no underlying cause for their headaches exists that should be addressed. In that regard, individuals should be alert for signs that their headaches may be more than merely a painful condition (e.g., their headaches are accompanied by numbness, blurred vision, dizziness, or memory loss; their headaches are getting stronger or are occurring more frequently).
8 Know thyself and thy triggers. Individuals should keep a lifestyle/activity diary on which they record information that could possibly help determine their personal triggers for their headaches. As such, they can try to identify any relationship between a specific factor and the onset of their headaches.
9 Age matters. Those who frequently have headaches are more likely to be younger (i.e., aged 34 years or younger) than older. In fact, children can have the same types of headaches as adults, including migraine and tension-induced headaches. However, once individuals reach the age of 65 years, they only have a 50% likelihood of having a single headache during the year compared with younger individuals.
10 Cold facts. Suffering a sudden headache after eating something very cold, such as ice cream, is fairly common-particularly among people who have a history of migraines. The best way to avoid “ice-cream headaches” is to eat the ice cream slowly to minimize the cold shock on the body.
The triggers for HA are different for each person. The best way to determine specific triggers is by keeping a HA diary and listing any activities or foods that help with or worsen a HA. It is a common misperception that HA is a sign of needing eyeglasses or a new prescription. This is true for some people, but not everybody. Others think that HAs are caused by high blood pressure. A HA with marked elevation in blood pressure is a symptom of a hypertensive crisis but is not associated with mildly elevated blood pressures. Although exercise may make some HAs worse, regular physical activity can help prevent HAs for some people. Because each person has a specific pattern of things that trigger or ameliorate his or her HA, it is important for people with recurrent HAs to consistently journal their specific HA modifiers. Recognition of HA patterns and modifiers is very important in HA management.

It is a common misconception that an HA is a sign of a brain tumor or aneurysm. People often think that a HA warrants immediate cerebral imaging with a magnetic resonance imaging scan or a computerized tomographic scan. Headaches are very common, as mentioned above, but HAs that need imaging are rare. However, any HA associated with dangerous signs, or “red flags,” does warrant further studies. This includes HA associated with nausea and vomiting, HA that worsens despite treatment, a change in the pattern of HA, and symptoms suggesting another medical condition. Other reasons for imaging include the “worst headache of (someone’s) life”; sudden onset of a severe persistent HA; HA associated with a fever or stiff neck; and HA with seizure, personality change, confusion, or loss of consciousness. Anyone with atypical symptoms also needs brain imaging.
Tension HA is the most commonly diagnosed form of HA. It has a distinct pattern of presentation. There are many different nonmedical therapies that are popular in the treatment of tension HA. Many people try massage, heat or water therapy, acupuncture, and botulinum toxin (Botox) injections. Some people with tension HA respond well to behavior modification techniques such as biofeedback and relaxation techniques

In contrast, people who have migraine HA do seek medical care. They are often thwarted in their search for a diagnosis and treatment. Many become frustrated and begin self-treatment after a few failures with traditional medicines. Unfortunately, the treatment of migraine HA is complex, with many different options. Because people respond to medicines differently, it may take months to develop an appropriate treatment regimen for a specific person.
The first step in the treatment of migraines is acute pain medicines. There are many different classes of medication available. As with any medication, it is important to treat until the pain is gone. Because migraines affect the mobility of the gut, nausea and vomiting are common symptoms associated with migraines. Reglan (metoclopramide) can help with gut symptoms.
By helping with gut motility, Reglan can increase the efficacy of other migraine medications. Acute treatment medications are available by both injection and nasal administration. Oral medications are still the most frequently prescribed and work well for most migraine sufferers. Migraines also seem to have the most diverse triggers. Keeping a concise diary of activity before a migraine can help determine a pattern of attacks and prevent future HAs.
Medications can help prevent problems and lost days of work if migraines occur two or more times per month, are associated with severe symptoms, require medication more than twice per week, do not respond to regular migraine treatment or are associated with neurological symptoms. Commonly used medications for the prevention of migraine include blood pressure medications such as β-blockers or calcium-channel blockers.

The antidepressant amitriptyline has shown good evidence for migraine prevention. There is less evidence supporting the use of fluoxetine, a selective serotonin reuptake inhibitor, but it is also commonly prescribed. Some physicians prescribe antiseizure drugs such as divalproex sodium and sodium valproate. The seizure medications have more untoward side effects than the other classes of medications, including anti-inflammatory medications. There are some studies demonstrating that naproxen and dihydroergotamine can prevent migraines without serious side effects.
There is a certain subtype of migraines called menstrual-related migraines (MRMs). These are similar to regular migraines but are triggered by menses. The treatment and prevention of this type of migraine are slightly different. Some women are better and some worse with hormonal treatment for MRM. There are some well-designed controlled studies demonstrating the efficacy of transdermal estrogen, or female hormone, for MRM.
Standard transdermal treatment or oral contraceptives are not indicated for the prevention of MRM because the decline in estrogen in the inactive pill week is equivalent to the decline experienced in the natural cycle, which is responsible for the MRM. Other studies show efficacy with triptans, specifically, sumatriptan, frovatriptan, and naratriptan. There are no studies that can demonstrate benefits with Naprosyn, although it is very frequently prescribed by primary care physicians for menstrual disturbances. Many women try natural remedies for their MRM HA, such as naturally occurring hormones.
There was one prospective randomized controlled study that negated the efficacy of phytoestrogens, or plant-based estrogen products, for MRM. Phytoestrogens are products available at natural supplement markets without prescription. Initial treatment of MRM should be the same as for migraine occurring at any time: a rapid-onset triptan administered early in the mild pain stage.
If MRM persists despite as-needed treatment, then treatment should address prevention. Prevention is best achieved with extended-cycle oral contraceptives, including transdermal estrogen, regular-cycle oral contraceptives with supplemental estrogen for the placebo days, or targeted supplemental estrogen. Treatment with hormonal supplements for MRM is no different from birth control and is not indicated for any woman older than 35 years who smoke. In addition, any use of estrogen is controversial in women with migraine associated with neurological symptoms. All women need to discuss the options available for treatment with their primary care provider.
In summary, keep in mind the warning symptoms for all forms of HA and immediately seek medical attention if indicated. Most HAs are diagnosed and treated at home. In people seeking medical attention, most will have migraine HAs. These are usually well treated with normal HA medication. If there is no response, there are some medications specific for migraine and some for the prevention of migraines.
References
1. Bajwa ZH, Sabahat A, Swanson JW. Preventative treatment of migraine in adults. Updated 2008 Aug [cited 2009 Jan]. Available from: http://www.uptodate.com/online/content/topic.do?topicKey=headache/2543&selectedTitle=2∼150&source=search_result.
2. Bigal ME, Serrano D, Reed M, Lipton RB. Chronic migraine in the population: Burden, diagnosis, and satisfaction with treatment. Neurology. 2008;71:559-66.
3. Bahra A, May A, Goadsby PJ. Cluster headaches: A prospective clinical study with diagnostic implications. Neurology. 2002;58(3):354-61.
4. Calhoun AH, Barbieri RL, Swanson JW. Estrogen-associated migraine. Updated 2008 May [cited 2009 Mar 4]. Available from: http://www.uptodate.com/online/content/topic.do?topicKey=gen_gyne/23264#2.
5. Bajwa Z, Wootton RJ. Evaluation of headache in adults. Updated 2008 Oct [cited 2008 Dec 24]. Available from: www.uptodate.com.
6. Modi S, Lowder DM. Medications for migraine prophylaxis. Am Fam Physician. 2006;73:72-80.
7. Silberstein SD, Rosenberg J. Multispecialty consensus on the diagnosis and treatment of headache. Neurology. 2000;54(5):1553.
8. Silberstein SD. Practice parameters: Evidence-based guide for migraine headache. Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2000;55(6):754-62.
9. Sierpino V, Astin J, Giordano J. Mind-body techniques for headache. Am Fam Physician. 2007;76:1518-24.
10. Snow V, Weiss K, Wall EM, et al. Guideline for the treatment and prevention of migraine headache. Ann Int Med. 2002;137:1-50.
https://journals.lww.com/acsm-healthfitness/Fulltext/2007/05000/Take_Ten__Take_and_Save__10_Nice_to_Know_Facts.18.aspx
https://journals.lww.com/acsm-healthfitness/Fulltext/2009/07000/Headaches__Common_Medical_Treatment.13.aspx






